Exosomes: Small Messengers with Big Potential
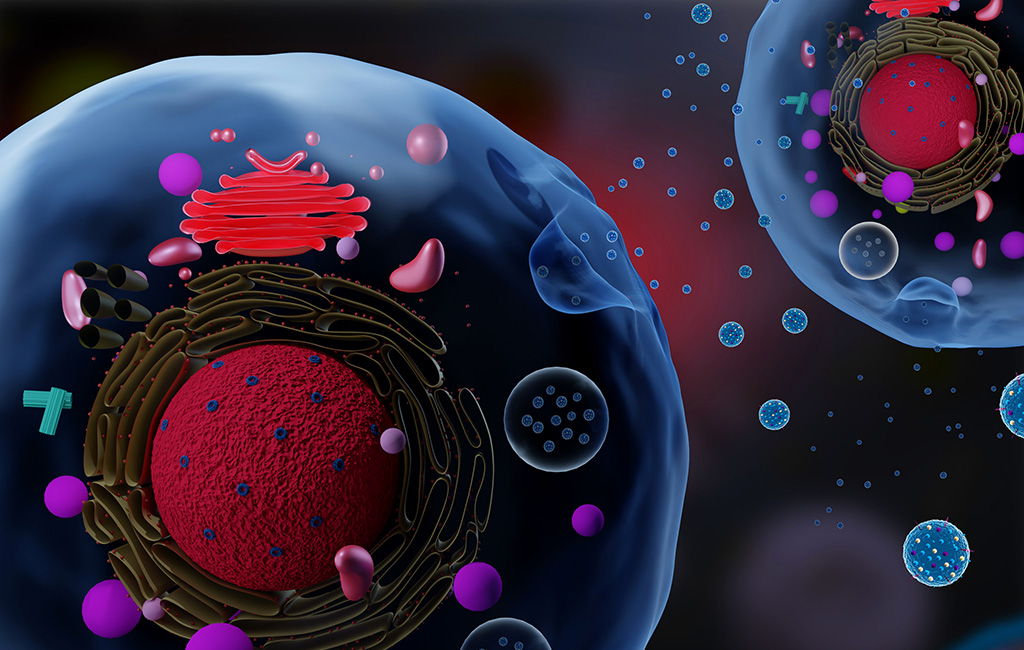
The cells in our body must constantly communicate with each other to keep physiological processes running smoothly. Extracellular vesicles are small, membrane-bound packages used by cells throughout the body to communicate across distances large and small. The composition of extracellular vesicles can vary greatly, and as such, they have been organized into 3 major groups according to their size, density, and origins. The smallest of these major three groups, exosomes, are a mere 30-150 nanometers wide. Yet despite their microscopic size, exosomes are potent carriers of information and capable of influencing immune responses, cell phenotypes, and tumor metastasis. As we improve our understanding of these important biological messengers, we have learned to leverage exosomes for both diagnostic and therapeutic purposes. In this article, we’ll discuss some of the promising advances that have been made using exosomes for cancer detection and treatment.
“Wait, that’s not junk mail”
Originally characterized in the mid-1980s, exosomes were once thought to be cellular trash bags. It was hypothesized that exosomes were simply an efficient way for cells to dispose of molecules and proteins that were no longer needed. However, as scientists continued to study these small vesicles, they realized exosomes were rather important messengers. Today, exosomes are better understood as small packages of information passed between cells, serving as powerful regulators in many key systems, as well as indicators of dysregulation in various disease states.
Several studies have demonstrated that exosomes alter immune activation states, driving both up and down-regulation of key processes such as inflammation, antigen presentation, and lymphocyte maturation. Exosomes perform these functions during normal immune responses, but these processes are also subverted by cancer cells. In fact, exosome levels have been shown to be increased in several types of cancers. Furthermore, researchers have determined that exosomes can transfer chemotherapy resistance between breast cancer cells, while other groups have shown that exosomes facilitate metastasis in both pancreatic and liver cancers. Given these discoveries, exosome depletion has been considered as a possible cancer treatment. Unfortunately, while exosome-targeting drugs showed some efficacy in mouse models, the non-specific nature of current compounds induced side effects that were too severe for use in clinical settings.
Reading the message: exosomes as diagnostics
While exosome depletion is not yet a viable treatment for cancer, exosomes’ relative abundance in biofluids has incredible diagnostic potential. Tissue collection is one of the predominant diagnostic tools for solid tumor cancers but faces several limitations. For instance, in cases of suspected cancer, it may not be feasible to obtain a sample of the tumor due to its location in the body or the health of the patient. Furthermore, information obtained from tumor biopsies is subject to sampling bias, as distinct regions of a tumor can express variations in gene expression, cellular morphology, metastatic potential, and other characteristics. Finally, the invasive nature of tissue biopsies is not suitable for routine cancer screening, which limits their applicability for early detection.
For these reasons, there is significant interest in the development and implementation of liquid biopsies, which use exosomes and DNA isolated from biological fluids to diagnose patients. Exosomes are packed with information that makes them an excellent target for diagnostic applications. For example, glypican 1 is a known surface protein found on exosomes associated with pancreatic and colon cancer. The lipid composition of exosomes can also be informative, as tumor-derived exosomes contain more phosphatidylserine (PS) on their surface than exosomes from non-tumor cells. And that’s just scratching the surface. When examining exosomal contents, such as miRNA, scientists have been able to predict how responsive patients would be to a given treatment. Exosomes are tightly compressed bundles full of valuable information, and as we continue to improve our ability to read these cellular messages, our ability to detect diseases will only grow.
Writing our own exosome messages
Exosomes can not only guide treatment regimens – they can be used as delivery vectors themselves. Biodegradable liposomes, such as poly-lactic-co-glycolic acid nanoparticles (PLGA-NPs) and poly-lactic acid nanoparticles (PLA-NPs), are frequently used for drug delivery. Exosomes represent an alternative delivery vector with several advantages over biodegradable liposomes. As a native biological structure, exosomes have increased biocompatibility and reduced toxicity compared to PLGA-NPs and PLA-NPs. Furthermore, exosomes are already designed to travel long distances within the body to reach specific tissues and cells, and as such, can be bioengineered to have superior cell-specificity and a prolonged half-life. Additionally, naturally occurring exosomes already exist that perform beneficial functions such as stimulating the immune response, aiding in antigen presentation, and generating antitumor responses.
Several clinical trials have already explored repurposing exosomes to package cancer treatments. One group has begun Phase I trials using plant exosomes to deliver curcumin, a potential anti-tumor agent, to the colon cells of cancer patients. Another current Phase II study seeks to use dendritic cell-derived exosomes to present tumor antigens as a cancer vaccination strategy. According to a September 2023 review, there are over 80 clinical trials in the United States exploring the use of exosomes for their diagnostic or therapeutic potential. The use of exosomes for therapeutics is a nascent field with exciting potential, as we learn to re-write exosomal messages to deliver potent therapies.
Finding the messenger: exosome isolation
One of the biggest barriers to increasing the use of exosomes in clinical settings is the isolation of these microscopic vesicles. In fact, there is currently no standardized protocol for isolating exosome particles, creating challenges with reproducibility and cross-study comparisons. Several commercial exosome isolation kits exist that achieve relatively pure isolation at the expense of higher yields. For higher yields, ultracentrifugation remains one of the primary isolation methods used by both clinicians and research laboratories. However, ultracentrifugation is a time-consuming process and can require additional purification steps to purify exosomes from co-precipitates, making it difficult to scale up across hospital systems. All current methodologies for exosome isolation face trade-offs between yield, specificity, time, and cost. More efficient isolation methods will be vital to fully realize the clinical potential of exosomes.
As we deepen our understanding of these small vesicles, we unlock substantial insights into how cells and tissues communicate with each other. By deciphering the intracellular messages carried by exosomes, we can learn to spot many diseases, including cancer, before serious symptoms develop, to empower earlier and more efficient treatments. Furthermore, these nanometer-sized packages can be repurposed to deliver diverse therapies, from small-molecule compounds to miRNA treatments. The diagnostic and therapeutic potential of exosomes is limited only by the tools and technologies we have to harness their power, but continued innovation in this space will undoubtedly drive future breakthroughs.
